ACREMONIUM
= Cephalosporium (Corda, 1839).
Pathogenicity
Acremonium
Acremonium has been reported as a rare cause of keratitis and endophthalmitis.
In the literature 17 cases of Acremonium keratitis have been reported between 1965 and 1991. Rosa et al (1994) found 3.2% of Acremonium keratitis in their series and Rodriguez-Areset al reported this as an extremely rare cause of suppurative corneal infection.
Ecology
Cosmopolitan, isolated from soil and plant debris.
MACROSCOPIC MORPHOLOGY
• The growth rate of Acremonium colonies is moderately rapid, maturing within 5 days. The diameter of the colony is 1-3 cm following incubation at 25°C for 7 days on potato glucose agar.
• The texture of the colony is compact, flat or folded, and occasionally raised in the center. It is glabrous, velvety, and membrane-like at the beginning. Powdery texture may also be observed. By aging, the surface of the colony may become cottony due to the overgrowth of loose hyphae.
• The color of the colony is white, pale grey or pale pink on the surface. The reverse side is either uncolored or a pink to rose-colored pigment production is observed (Fig. 8.1).
MICROSCOPIC MORPHOLOGY
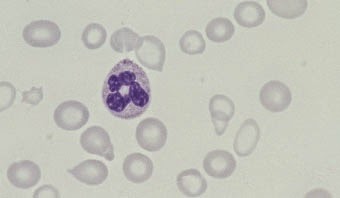
• Acremonium spp. possesses hyaline, septate hyphae which are typically very fine and narrow. Vegetative hyphae often form hyphal ropes. Unbranched, solitary, erect phialides are formed directly on the hyphal tips, the hyphal ropes, or both. The phialides are separated from hyphae by a septum and taper towards their apices. At the apices of the phialides is the hyaline conidia 2-3 × 4-8 μm in size. They usually appear in clusters, in balls or rarely as fragile chains.
• The conidia are bound by a gelatinous material. They may be single or multicellular, fusiform with a slight curve or resemble a shallow crescent. These structural properties of conidia vary depending on the species.
• Acremonium falciforme usually produces crescentic, nonseptate conidia. Sometimes, 2 or 3 celled conidia may also be observed. Acremonium kiliense, on the other hand, has short straight conidia and the conidia of Acremonium recifei are usually crescentic and nonseptate (Figs 8.1 and 8.2).
 |
| Fig. 8.1: Acremonium species on potato dextrose agar, 25°C, 7 days |