Red cells should be assessed as to their:
• number
• size
• shape
• degree of haemoglobinization
• distribution in the blood film.
Their appearance should be described using a standard terminology.
Assessing red cell number and distribution (anaemia, polycythaemia, rouleaux formation, red cell agglutination)
The thickness of a film of blood spread on a glass slide is deter- mined by how thick the blood is, i.e. by its viscosity. This in turn is determined by the Hb. In a normal blood film it is possible to find a part of the film which is ideal for microscopic examination where the red cells are touching but not overlapping. If the Hb is abnormally high (a condition referred to as polycythaemia) the blood has a high viscosity and the film of blood on the glass slide is thick. The red cells therefore appear packed together through- out the whole length of the film. The term ‘packed film’ is often used. Conversely, when a patient is anaemic the viscosity of the blood is low, the blood film is very thin and there are large spaces between the red cells. The effect of Hb on the blood film can be seen by comparing Figs 2.1, 2.2 and 2.3.
Usually red cells are distributed fairly regularly on the slide. Two abnormalities of distribution may occur. When there is an
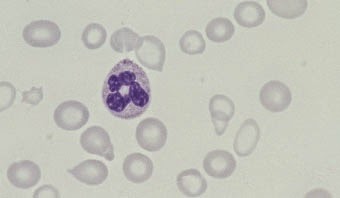 |
Fig. 2.1 Anaemia (caused
by iron deficiency).
|
 |
| Fig. 2.2 Normal distribution of red cells in a healthy subject with normal Hb |
 |
Fig. 2.3 Polycythaemia.
|
increase in high-molecular-weight plasma proteins there is an effect on the electrical charge on the surface of the red cells and the cells sediment rapidly and form into stacks, like a pile of coins. These stacks are referred to as rouleaux (Fig. 2.4) and the film is said to show increased rouleaux formation. The other abnormality of cell distribution is red cell agglutination. This is caused by an antibody against a red cell antigen. The antibodycoated red cells become sticky and form into irregularly shaped
 |
Fig. 2.4 Rouleaux.
|
 |
Fig. 2.5 Red cell agglutinates.
|
clumps or agglutinates (Fig. 2.5). Agglutinates can be distin- guished from rouleaux because the clumps are an irregular jum- ble rather than an orderly stack. Red cell agglutinates are most often caused by an antibody which is active below normal body temperature, referred to as a cold antibody or cold agglutinin. Agglutinates will be less numerous if another film is made after the blood has been warmed. The presence of cold agglutinins can lead to anomalous blood count results.
Assessing red cell size (microcytosis, macrocytosis, anisocytosis)
Red cells are smaller than normal lymphocytes and significantly smaller than granulocytes. If cells are smaller than normal they are described as microcytic and if larger than normal as macro- cytic. They are referred to as microcytes or macrocytes respec- tively. Red cells of normal size are said to be normocytic. If red cells show greater variation in size than normal the blood film is said to show anisocytosis (Fig. 2.6). Anisocytosis can be graded as +, ++ or +++ (mild, moderate or severe). The different sizes of red cells can be appreciated by comparing Figs 2.7, 2.8 and 2.9.
 |
| Fig. 2.6 Severe anisocytosis; the MCV was 133 fl but the macrocytosis is not uniform |
Assessing red cell shape (poikilocytosis)
If red cells show more than the normal degree of variation in red cell shape there is said to be poikilocytosis (Fig. 2.10).
 |
| Fig. 2.7 Microcytic red cells (MCV 62 fl) |
 |
Fig. 2.8 Normocytic red cells.
|
..jpg) |
Fig. 2.9 Macrocytic red cells (MCV
105 fl).
|
 |
| Fig. 2.11 Diagrammatic representation of different types of poikilocyte |
Individual cells of abnormal shape are referred to as poikilocytes. Poikilocytosis can be graded in a similar manner to anisocytosis. Individual cells of a particular shape have names which identify them, as defined in Table 2.1 and illustrated in Fig. 2.11 and Figs 2.12–2.22.
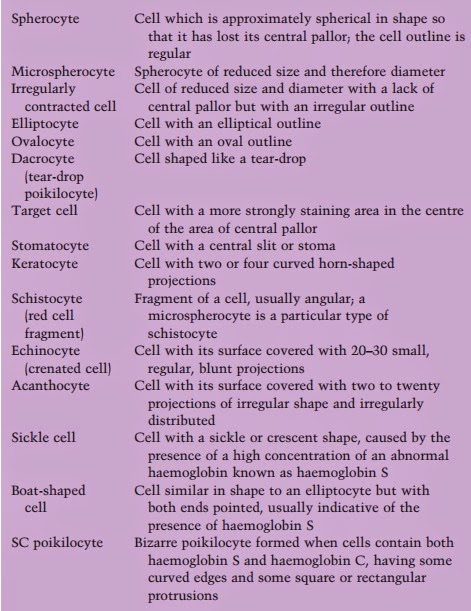 |
Table 2.1 Definitions of cells by shape.
|
..jpg) |
Fig. 2.12 Moderate numbers of spherocytes (in hereditary spherocytosis).
|
.%2BThe%2B%2Bmajority%2Bof%2Bthe%2B%2Bother%2Bcells%2B%2Bare%2Btarget%2Bcells..jpg) |
Fig. 2.13 Several irregularly contracted cells (in haemoglobin C
disease). The majority of the other cells are target cells.
|
..jpg) |
Fig. 2.14 Numerous elliptocytes and ovalocytes (in hereditary
elliptocytosis).
|
%2B(in%2Bidiopathic%2Bmyelo%EF%AC%81brosis)..jpg) |
Fig. 2.15 Several dacrocytes (tear-drop poikilocytes) (in idiopathic myelofibrosis).
|
..jpg) |
Fig. 2.16 Numerous stomatocytes (in hereditary stomatocytosis).
|
 |
| Fig. 2.17 Several keratocytes (in microangiopathic haemolytic anaemia); keratocytes are sometimes called ‘bite cells’ because they look as if a bite has been taken from them. |
 |
| Fig. 2.18 Several schistocytes (red cell fragments) including a microspherocyte (in haemolytic uraemic syndrome). |
 |
Fig. 2.19 Echinocytes (crenated
cells) (in
chronic renal failure).
|
..jpg) |
Fig. 2.20 Acanthocytes (in abetalipoproteinaemia).
|
..jpg) |
Fig. 2.21 One sickle cell
and
several boat-shaped cells (in sickle cell anaemia).
|
 |
Fig. 2.22 SC poikilocytes (in sickle cell/haemoglobin C disease).
|
Assessing red cell colour (hypochromia, hyperchromia, anisochromasia, polychromasia)
Normal red cells are reddish-brown with approximately the cen- tral third to quarter of the cell being paler. They are described as
 |
Fig. 2.24 Normochromic cells (in a healthy subject).
|
 |
| Fig. 2.25 Hyperchromic cells (which in this case are microspherocytes in a severely burned patient; spherocytes and irregularly contracted cells are also hyperchromic). |
 |
| Fig. 2.26 A polychromatic macrocyte |
normochromic. Cells which have an area of central pallor more than a third of the diameter of the cell are said to be hypochromic and the film is said to show hypochromia. Cells which lack central pallor are said to be hyperchromic. Hypochromic, normo- chromic and hyperchromic cells are compared in Figs 2.23–2.25. These staining characteristics are determined by the concentra- tion of haemoglobin in the cell and by the shape of the cell. Cells which show a greater than normal variation in the degree of haemoglobinization are said to show anisochromasia (see Fig. 2.1). Red cells which have a blue or lilac tinge are said to show polychromasia (‘many colours’). Polychromatic cells (Fig. 2.26) are young cells, newly released from the bone marrow. They have not yet been remodelled to the disc shape of a mature erythrocyte and therefore lack central pallor. They are also gen- erally larger than more mature cells and in this case may be described as polychromatic macrocytes. Young red cells can also be detected with a special stain of live (unfixed) cells called a supravital stain. Young cells detected in this way are called reticulocytes because the supravital staining causes a network or ‘reticulum’ to be deposited. Another word usually used to de- scribe staining characteristics of red cells is dimorphic. The word means that there are two types of cell but it is most often applied to a mixture of hypochromic and normochromic cells (see Fig. 2.23). The two populations of cells usually differ in size as well as in staining characteristics. A dimorphic film differs from
 |
| Fig. 2.27 Numerous cells showing basophilic stippling (in lead poisoning). Punctate basophilia is an alternative term used to describe this abnormality. |
one showing anisochromasia in that there are two distinct populations of cells rather than a gradation of staining character- istics.
Detecting red cell inclusions (Pappenheimer bodies, basophilic stippling, Howell–Jolly bodies)
Red cells may contain inclusions. Pappenheimer bodies are small, basophilic inclusions, occurring in small numbers to- wards the periphery of the cell (see Fig. 2.23). They contain iron and when this is confirmed by an iron stain they are referred to as siderotic granules. Basophilic stippling refers to the presence of small basophilic inclusions distributed throughout the red cell (Fig. 2.27). They do not contain iron but represent abnormally staining ribosomes. Howell–Jolly bodies (Fig. 2.28) are larger, round, densely staining inclusions, usually towards one edge of the cell. They represent a nuclear fragment that was not extrud- ed when the red cell left the bone marrow. Usually any Howell– Jolly bodies left in red cells as they leave the bone marrow are removed by the spleen. They are therefore most often seen in people who have had their spleens removed. Malaria parasites are intracellular and are detected as inclu- sions within red cells. Their detection is very important in diag-
 |
| Fig. 2.28 A cell containing a Howell–Jolly body in a patient who has had a splenectomy. There are also several target cells. |
nosis and as yet there is no reliable substitute for the blood film in their detection.
The full blood count in red cell assessment
The blood count is very important in detecting or confirming the presence of anaemia, polycythaemia, microcytosis and macro- cytosis. Some instruments also detect hypochromia and hyper- chromia by changes in the MCHC. Most instruments can detect the presence of two cell populations which would produce a dimorphic blood film. Many instruments also produce a meas- urement called the red cell distribution width (RDW), which quantitates anisocytosis. Some also produce a measurement called the haemoglobin distribution width (HDW), which is in- dicative of the degree of anisochromasia. The adequate assessment of an abnormal blood count often requires the examination of a blood film since there are many abnormalities detectable on blood films which are not detected by automated counters, e.g. the presence of poikilocytes, red cell inclusions or increased rouleaux formation. The presence of red cell agglutinates can sometimes be suspected because of very abnormal and improbable FBC results but a blood film is needed for confirmation.



No comments:
Post a Comment